Hypertrophic Cardiomyopathy (HCM)
Summary:
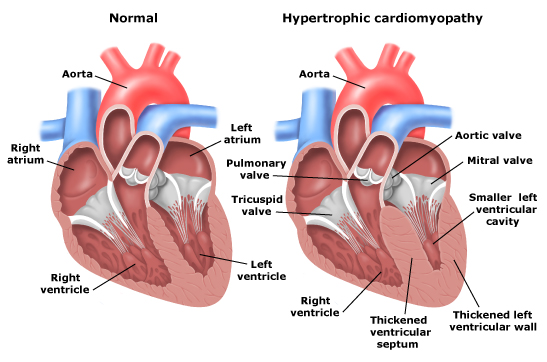
HCM is a condition that interferes with the blood flow out of the heart, and is the most common heart-related cause of sudden death during intense exercise. It’s caused by abnormal growth of the muscle cells that make up the heart wall, which makes the heart wall thicker and reduces the heart’s ability to pump properly. Treatment options include implanted pacemakers to help the heart maintain a normal rhythm, and in some cases operations to reduce the obstruction to blood flow.
Technical overview:
HCM is a condition that affects heart muscle cells and is characterised by some parts of the heart wall being thicker than normal, typically these changes do not appear symmetrical. Histology (microscopic examination of heart muscle) frequently shows myofibril disarray, this is when the regular orientation of individual muscle fibres is disturbed. HCM affects between 1 in 500 to 1 in 200 in the general population (Semsarian 2015) and most people live normal lives. Sometimes the muscle thickening can obstruct the bloodflow out of the heart and corrective surgery may be necessary. Sudden death from heart arrhythmias, often during exercise, occurs in about 1% of affected people.
Features such as a family history of premature death, excessive thickness of the interventricular septum and asymptomatic ventricular arrhythmias identify a subset at higher risk of cardiac arrest and a preventative placement of an implantable defibrillator is recommended in such cases.
Management:
The diagnosis of HCM is best made by performing a ultrasound of the heart, usually by echocardiography, although magnetic resanance imaging (MRI) contributes additional useful information and both tests are recommended. The 12 lead ECG is abnormal in 80% of cases and exercise testing to measure the blood pressure resoponse and 24 hour ambulatory monitoring to detect arrhythmias are also appropriate. Atrial fibrillation, when the heart rhythm becomes irregular, is an important complication occuring in about 25% of people. Strenuous efforts should be made to restore normal rhythm, with medication, cardioversion and occasionally ablation (burning or freezing of electrical pathways in the heart). HCM may not be evident from the first lot of tests as it is a condition that can progress with age. Therefore we would advise that interval testing should be performed every few years.
Inheritance and genetics:
About 50% of cases are familial, though this may well be an underestimate, with an autosomal-dominant pattern of inheritance. HCM is caused by mutations in 11 or more genes encoding thick and thin contractile myofilament protein components of the sarcomere or adjacent Z-disc (cells of the heart muscle). However a disease causing gene mutation is only found in about 50% of clearly affected individuals, suggesting there are relevant genes yet to be identified. About 70% of genetically tested patients have mutations in the 2 most common genes, beta-myosin heavy chain and myosin-binding protein C. To date, more than 1,500 individual gene mutations have now been been found [Maron 2015) Individuals with the same mutation may have very different degrees of hypertrophy , which is termed “variable penetrance”.
The outlook for diagnosed patients is now very good and the great majority of people can expect to live normal lives.
Further information and lay summaries are available at the Cardiomyopathy Association of Australia