Genetic testing (from a blood sample) can be useful, see below. It takes between two and three months to get a result.
Who is at greatest risk?
Risk varies by the type of long QT syndrome, the presence of symptoms, age, sex and the length of the QT interval.
Those at greatest risk are those with a very long QT interval who have had a sudden loss of consciousness. Boys and women tend to have higher risk than men and girls.
Treatment and outlook (prognosis)
Risk can be effectively managed in LQTS, and in general, patients who follow treatment recommendations can expect to do very well.
- Everyone must avoid a list of medications which are known to prolong the QT interval. You can also see our list of Medications to Avoid in Long QT Syndrome A constantly updated list is found at www.crediblemeds.org, it takes 2 minutes to register.
- Everyone with a history of sudden loss of consciousness and those with a long QT interval should take a beta blocker medication regularly. An example is Nadolol (a tablet taken once a day), and in young children, liquid atenolol taken at least twice a day.
- People with the most severe forms, or who cannot take beta blockers, can benefit from a key-hole surgery where the nerves to the heart from the neck on the left side are cut, called a left cardiac sympathectomy. While very effective, this has side effects which need careful consideration.
- Those who have survived a cardiac arrest, or have an extremely severe rare form of LQTS, may benefit from an implanted defibrillator pacemaker.
Lifestyle restrictions
Aside from avoiding some medications, these are few, but they are tailored to each person’s risk as assessed by their cardiologist.
People with long QT type 1, especially boys with a long QT interval, need to be very careful in water, since a momentary loss of consciousness in water results in drowning. In general they should avoid swimming where possible, although those with mild disease and taking beta blockers consistently are relatively safe in a pool provided they are watched carefully by someone who can rescue them.
People with long QT type 2 should try to minimise loud noises at night. (Remove that loud alarm clock!)
American Heart Association guidelines suggest quite rigid restrictions on sporting activities, but recent evidence suggests that these are unnecessarily restrictive. Adherence to beta blocker medication is the most reliable key to safety. Discuss these things with your own cardiologist.
Genetics
As of 2015, we know of 16 genetic types of LQTS. However, the vast majority are types 1, 2 and 3. The others are mostly very rare. In about 25% of cases we have yet to find the gene involved. Each type has its own characteristics, and each is linked to a particular gene. These genes control the make-up of the channels which move potassium and sodium across the heart cell walls (the “cardiac ion channels”). Each can affect both males and females. When someone with the gene has children, on average half of the children will also carry it; it is rather like flipping a coin. Similarly, only one of the patient’s parents may have the gene.
- LQTS type 1 (affects 50% of carriers) The gene is KCNQ1. Affects boys mostly. Sudden loss of consciousness often occurs with exercise, especially swimming.
- LQTS type 2 (affects 40% of carriers). The gene is KCHN2. Affects women mostly. Sudden loss of consciousness classically follows a startle, or a loud noise at night. Seizures or sudden death at night may occur.
- LQTS type 3 (affects 10% of carriers). The gene is SCN5A. Death or seizures may occur during sleep, typically in adult males.
Genetic testing can only be done through a genetic service, such as CIDG, or the national clinical genetic service. It is not available to GPs and general cardiologists or paediatricians. The main use of genetic testing is to help decide who within a known affected family is carrying the condition. It is used in addition to the ECG.
Doctor Talk
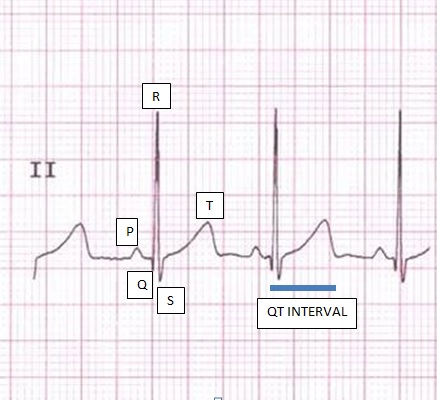
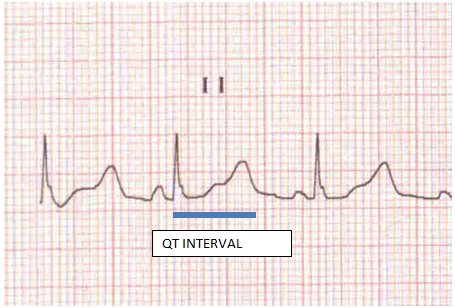
LQTS is characterised by abnormally prolonged ventricular repolarisation due to defects in cardiac ion channels. Prolongation of ventricular repolarisation is shown on the surface electrocardiogram (ECG) by prolongation of the interval between the onset of the Q wave and end of the T wave. The condition predisposes affected people to ventricular tachyarrhythmias particularly Torsades de Pointes. This may lead to sudden loss of consciousness or sudden death, most commonly with exercise or stress, but also at times of rest.
Those affected are almost always outwardly normal, active members of society.
Since the loss of consciousness may be associated with a seizure, misdiagnosis of LQTS as epilepsy is common. This can dangerously delay diagnosis for many years [McCormick 2009]. Drowning in a strong swimmer is likely to be due to LQTS (or CPVT- see below). Death due to long QT syndrome during rest or sleep tends to occur in women with long QT type 2 and males with long QT type 3. LQTS is inherited as an autosomal dominant condition, with 16 candidate genes currently identified. Thus it affects males and females. There are thousands of mutations within these three common genes, some mutations are more malignant than others. Many families have a mutation which is unique to them.
Genetics
Each offspring of someone with LQTS has a 50% chance of carrying the abnormal genetic mutation. However more than half of gene carriers will never have a symptom due to LQTS. Those at greatest risk are gene carriers who have already experienced a sudden collapse, and those with a very long QT interval on their ECG.
A family history of sudden death in a close relative does not per se imply a high risk. Predominantly, mutations in three genes encoding proteins of cardiac potassium and sodium ion channels have been identified: KVLQT1 (KCNQ1), HERG (KCNH2), and SCN5A which account for ~ 40%. 30% and 10% of cases respectively. Approximately 75-80% of known families have identified mutations. The frequency of LQTS may be greater than 1/2000 of the population.
In New Zealand, mutations within KCNQ1 predominate (57%), followed by KCNH2 (28%) and then SCN5A (15%). SCN5A mutations have mostly been identified from sudden death or “near miss” victims. Genetic diagnosis now plays a pivotal part of management and counselling of these families. Clinical diagnosis in family members may be uncertain in as many as 30%. In families where a mutation has been identified, 30% of mutation carriers can have an electrocardiogram which has a QT interval in the normal range. The problem is that QT intervals can be quite long in the normal population and the overlap with long QT gene carriers is considerable (Viskin 2009). Those with a normal QT interval are, nevertheless, at risk for adverse cardiac events. It is certainly important to have more than one ECG in borderline cases, and exercise testing can help make the abnormalities more obvious.
Administration of beta blocker medication reduces the chance of sudden death by 50-75%, possibly more if we can assure adherence. Other effective strategies include avoidance of triggers linked to the genotype (such as swimming in long QT 1,and loud alarm clocks with long QT 2), avoidance of certain medications (listed on crediblemeds.org), and in a minority, defibrillator pacemakers or left cardiac sympathectomy. This procedure is done thoracoscopically in specialist centres; it is the same procedure used to treat hyperhidrosis of the hands.
Measurement of the QT interval
This is often done badly, and repeatability between doctors is famously very poor. Automated measurements on ECG machines are unreliable.
Measure the QT interval in both leads 11 and V5. Take the onset of Q wave to end of the T wave defined by the intersection of the tangent of the steep slope of the T wave with the baseline. Divide this by the square root of the preceding R-R interval. Use the larger of the two values. This value should, in general, be less than 470ms in women and 450ms in men, but there is considerable overlap with normal and LQTS patients. In asymptomatic, non-familial cases, a diagnosis of LQTS can only be made with confidence with a QTc of 500ms or greater on two ECGs.
Note that the appearance of the T wave is also important. It tends to be broad in LQTS type 1, and have a double bump in type 2. In children, ignore the precordial leads V 1 to V4 which can look quite strange even in non LQTS subjects.
Treatment
Treatment is basically in four levels with escalating severity of disease:
- Avoiding QT prolonging medications (crediblemeds.org)
- Beta blockers long-term
- Left Cardiac Sympathectomy
- Implantable cardioverter defibrillators